What is Fibromyalgia and how do you know you have it?
Fibromyalgia, often embodied in the collective memory as an elusive condition, is characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory, and mood issues. Imagine you've just spent the day gardening or performing a task you're not accustomed to, and the next day, your body aches all over. Now, imagine feeling that way most of the time without any apparent reason. This is a glimpse into what fibromyalgia sufferers might experience.
History of the condition known today as Fibromyalgia
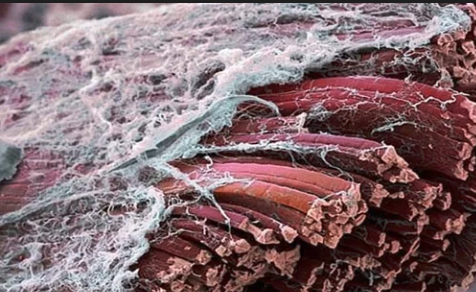
The term "fibromyalgia" is derived from a combination of Latin and Greek words: "fibro-" refers to fibrous tissues (such as tendons and ligaments), "myo-" means muscle, and "algia" signifies pain. Thus, "fibromyalgia" translates to "pain in the muscle and fibrous tissues."
This name reflects the condition's hallmark symptom of widespread musculoskeletal pain, along with other symptoms such as fatigue, sleep disturbances, and cognitive difficulties. The term was adopted to describe the syndrome in the early 1990s, succeeding previous names like "fibrositis." The earlier term implied inflammation (-itis) of the muscular and fibrous tissue, which is not a characteristic of fibromyalgia, as it does not involve inflammation of the tissues. The shift in terminology to "fibromyalgia" better encompasses the nature of the condition, focusing on pain without suggesting inflammation, thus more accurately describing the disorder's characteristics.
Etiology
The exact cause of fibromyalgia remains a puzzle, but it's thought to involve a variety of factors working together. These may include genetics, as fibromyalgia tends to run in families; infections, which may trigger or exacerbate the condition; and physical or emotional trauma, where post-traumatic stress disorder (PTSD) has been linked to fibromyalgia. Researchers believe these factors may lead to a change in the way the brain and spinal cord process pain signals, amplifying painful sensations (a phenomenon known as abnormal pain perception processing).
Common Signs and Symptoms
Fibromyalgia is known for widespread pain, described as a constant dull ache that has lasted for at least three months. To be considered widespread, the pain must occur on both sides of the body and above and below the waist. Other common symptoms include:
- Fatigue, even after sleeping for long periods
- Sleep disturbances
- Cognitive difficulties, often referred to as "fibro fog," impairing the ability to focus, pay attention, and concentrate on mental tasks
- Headaches, including migraines
- Depression and anxiety
Affected Population
Fibromyalgia affects millions worldwide, with a notable prevalence among women. Though it can occur at any age, it is most commonly diagnosed in middle age and the risk increases with age. It can also coexist with other painful conditions, such as irritable bowel syndrome, migraines, and arthritis.
How Fibromyalgia was first diagnosed – an emphasis of tenderness/ pain
The concept of tender points is central to older diagnostic criteria for fibromyalgia, developed by the American College of Rheumatology (ACR) in 1990. These criteria identified 18 specific tender points on the body that were used to diagnose fibromyalgia. For a diagnosis, patients had to have widespread pain and tenderness in at least 11 of these 18 points when a specified amount of pressure was applied.
The 18 tender points are located at specific sites, including:
- Front Lower Sides of the Neck: Just above the collarbone on either side of the larynx.
- Back Lower Sides of the Neck: Where the neck muscles attach to the base of the skull.
- Upper Chest: Just below the collarbone, near the second rib.
- Elbows: Near the elbow, on the outer sides where the forearm muscles attach.
- Upper Back: In the trapezius muscle, midway between the neck and shoulder.
- Shoulders: At the top of the shoulder, just above the scapula (shoulder blade).
- Upper Buttocks: In the upper outer quadrants of the buttocks.
- Hips: On the side, near where the buttock muscles curve to join the thighs.
- Inner Knees: On the fat pad just above the joint line.
These points were used as a tool in the assessment of fibromyalgia, but the reliance on tender points for diagnosis has decreased over time. In 2010, the ACR introduced new diagnostic criteria that no longer require a physical examination of tender points. Instead, these criteria focus on the extent of widespread pain and the severity of symptoms such as fatigue, waking unrefreshed, and cognitive (memory or thought) difficulties. This shift acknowledges the variability in symptoms among fibromyalgia patients and the complexity of the condition, which cannot be fully captured by the presence or absence of pain at specific points.
Despite the evolution in diagnostic criteria, understanding tender points remains a part of the historical context of fibromyalgia diagnosis and provides insight into the condition's characterization as involving widespread pain and sensitivity.
How do doctors today determine if you have fibromyalgia?
Diagnosing fibromyalgia can be a complex process, primarily because there is no specific laboratory test or imaging scan that definitively diagnoses the condition. For many years, doctors relied on a widespread pain index and symptom severity scale, along with a physical examination. The criteria included a history of widespread pain lasting at least three months and the presence of other symptoms such as fatigue, waking up tired, and cognitive (memory or thought) problems. In the past, some clinicians used a tender point exam, requiring pain in at least 11 of 18 specific points on the body, but this method is less commonly used today due to its subjectivity.
Medical Tests and Blood Tests
While no test can directly diagnose fibromyalgia, doctors may order a series of blood tests to rule out other conditions that may have similar symptoms. These tests include:
- Complete blood count (CBC): To check for signs of anemia or other abnormalities that could explain fatigue and other symptoms.
- Erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP): These tests measure inflammation in the body, which might indicate conditions such as rheumatoid arthritis.
- Thyroid function tests: To ensure the thyroid gland is working correctly, as thyroid issues can mimic fibromyalgia symptoms.
- Rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies: To rule out rheumatoid arthritis.
- Antinuclear antibody (ANA): To check for autoimmune diseases.
These tests help exclude other conditions like lupus, rheumatoid arthritis, and other autoimmune diseases, which can present with widespread body pain and fatigue similar to fibromyalgia. After other conditions are ruled out, and the patient's symptoms align with fibromyalgia criteria, a diagnosis may be made based on clinical evaluation.
The reality of diagnosing Fibromyalgia
The diagnosis of fibromyalgia is largely a process of elimination, combined with a detailed examination of the patient's medical history and symptoms. It's essential for patients to communicate all their symptoms comprehensively to their healthcare provider to aid in the diagnostic process. Even though the path to a fibromyalgia diagnosis can be frustrating due to the lack of a simple test, it's an important step towards managing symptoms and improving quality of life.
Current Medical/Pharmacological Treatments
There is no cure for fibromyalgia, but medications can help manage symptoms. Treatment often includes pain relievers, antidepressants, and anti-seizure drugs. Pain relievers, both over-the-counter (such as acetaminophen, ibuprofen) and prescription, are commonly used. Antidepressants can help ease pain and fatigue, while anti-seizure drugs, originally developed for epilepsy, may reduce certain types of pain.
Alternative Treatments
Many individuals find relief through alternative or complementary treatments, including:
- Physical therapy to improve strength, flexibility, and stamina
- Acupuncture, which may help relieve pain for some
- Massage therapy to reduce muscle tension and stress
- Yoga and tai chi, which combine meditation, slow movements, deep breathing, and relaxation
There is currently an interest in using Pulsed EMF to help manage fibromyalgia. The classic presentation of fibromyalgia—perceived widespread, diffuse pain throughout the musculoskeletal system absent of a definitive, measurable pathology via physical exam, imaging studies or blood and urine studies suggests dysfunction within the central nervous system (brain, brainstem, and spinal cord). Neurons are the special cells that comprise central nervous system tissue, and it is possible that the perception of pain may be related to abnormal neuron firing. Neurons transmit bioelectrical signals to one another, and eventually to tissues. This is a big part of how the body regulates itself. Signals going from body to brain are sensory impulses, while signals from brain and spinal cord to body are motor impulses.
Since this depolarization is achieved by flow of ions across the membranes of neurons, any problem associated with the movements of these ions can theoretically result in abnormal sensations, including pain. Pulsed EMF is a modality that uses electromagnetic fields at low frequency to influence the movement of charges in tissues. In the case of fibromyalgia, it may be worthwhile to try a regimen of Pulsed EMF treatment, targeting the brain and spinal cord. If the source of pain in fibromyalgia is related to abnormal membrane polarization in neurons of the central nervous system, it may be possible to correct, or alleviate the problem using pulsed EMF.
Lifestyle adjustments and self-care are critical components of managing fibromyalgia. Regular exercise, stress-reduction techniques, and good sleep hygiene practices can significantly impact the severity of symptoms and overall quality of life.
Conclusion
The journey of understanding and managing fibromyalgia is ongoing, with research continuously uncovering new aspects of the condition and its treatment. Patients are encouraged to work closely with their healthcare providers to find a treatment plan that addresses their symptoms and improves their quality of life.
